Gut-Brain Connection: How Your Digestion Impacts Your Mental Well-being
A direct gut-brain relationship has been found to exist; one such examples incorporates the production of the neurotransmitter serotonin by the gut.
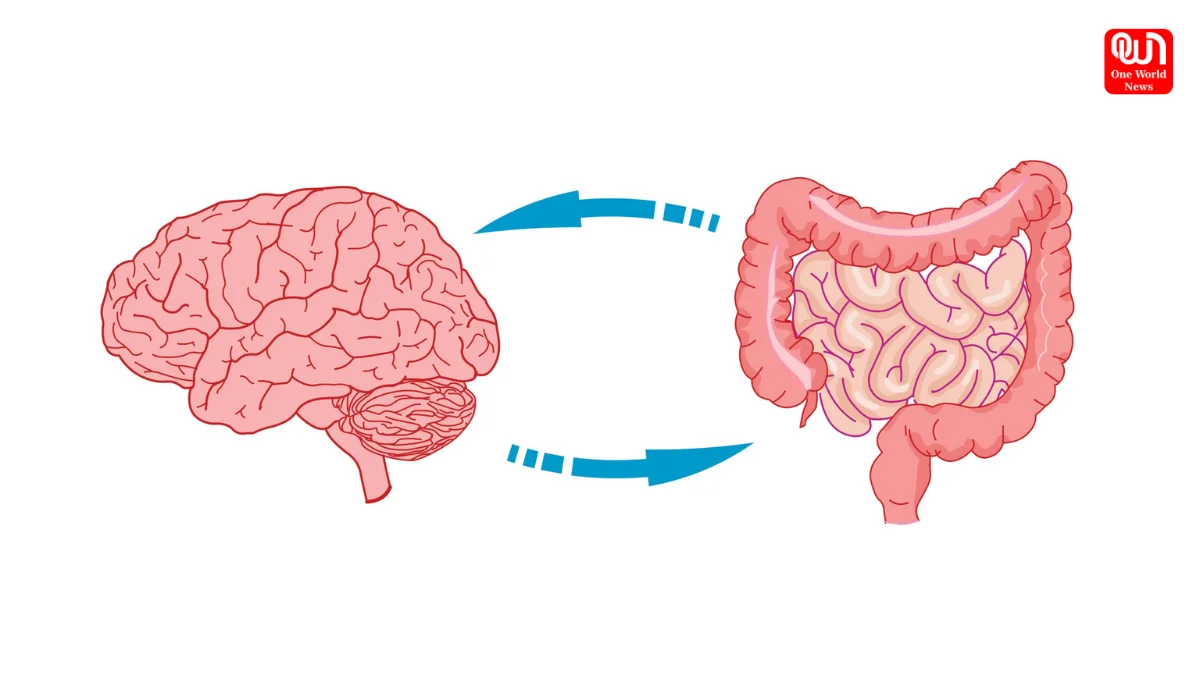
The Gut-Brain Axis: A Two-Way Street
A direct gut-brain relationship has been found to exist; one such examples incorporates the production of the neurotransmitter serotonin by the gut. It has been well studied and understood that the gut is one of the largest producing organs for serotonin, amine hormone known for grappling with the regulation of sleep, mood, and appetite. Most of the body’s serotonin is estimated to be synthesized in the gut. When there is an imbalance in gut microbiome, which is known as dysbiosis, it disrupts this very important production; depletion of serotonin may cause triggering or aggravating the onset of mood disorders like anxiety and depression. The gut also produces dopamine, which is pleasure and motivation aligned, another important neurotransmitter, and gamma-aminobutyric acid (GABA), which has a calming effect.
The Vagus Nerve: A Direct Line of Communication-
A long and extensive nerve extending from the brainstem up to the abdomen and serving as communications between the two organs is the vagus nerve. It forms the major bidirectional highway between the gut and the brain. Signals originating from the gut, according to composition and metabolic activities of the gut microbiome, are amalgamated down via the vagus nerve toward the brain to affect brain fuctioning plus emotion processing; on the other hand, the brain signals can also shoot down the vagus nerve to the gut whereby motility, secretion, and even balance of the gut microbiome changes could manifest. Examples of effect would be changes in gut function, such as bowel habit changes with stress, highlighting this dual communication.
Inflammation and Gut Microbiome Role-
Trillions of these microorganisms make up the gut microbiome, which is critical to the promotion of overall health, including mental health. Such microbes might be defined as fermenting fibers from food and producing short-chain fatty acids (SCFAs), which carry anti-inflammatory properties and might alter brain functioning. However, with an imbalance in the gut microbiome, increased intestinal permeability (leaky gut) and a systemic inflammatory response can result. Under such conditions, especially chronic low-grade inflammation, the incident may show rising association with the pathogenesis of many mental health-related disorders, including depression, anxiety, and even diseases like Alzheimer’s and other neurodegenerative types.
Clinical Evidence: Gut Disorders and Mental Health
Clinical observations and research studies show, by-and-large, that anxiety and depression are more prevalent in individuals with gastrointestinal disorders such as Irritable Bowel Syndrome (IBS) and inflammatory bowel diseases (IBD). This co-occurrence strengthens the understanding of the gut-brain axis even further. Emerging research is also looking at modulating the gut microbiome, with interventions like probiotics (live beneficial bacteria) or prebiotics (the dietary fibers that encourage the growth of beneficial bacteria), which may hold therapeutic value in mental health. Some studies have suggested that microbial interventions are promising in reducing symptoms of anxiety and depression.
The Gut Microbiome and the Stress Response System-
The gut microbiome can in turn have effects upon the body’s central stress response system, which consists of the hypothalamic-pituitary-adrenal (HPA) axis. An imbalanced gut microbial community could cause an overactive HPA axis, increasing the levels of stress hormones such as cortisol. When the brain is under constant exposure to elevated levels of cortisol, it suffers harmful effects, and the vulnerability to depression and other diseases becomes greater. A well-balanced gut microbiome therefore can possibly be involved in modulating the stress reactions in the body thereby providing resistance.
Read More: Endometriosis and Pregnancy: Essential Facts Every Woman Should Know
In sum, the link connecting gut health and mental health constitutes a complex and bidirectional relationship with implications for the farthest reaches. Fostering a healthy and diverse gut microbiome through a balanced diet, rich in fiber and fermented foods, practicing good stress management, and investigating well-placed examples of prebiotics and probiotics could provide us meaningful avenues for support to our physical health and mental well-being. Clearily the potential for a defined therapeutic approach aimed at the gut to change mental health outcomes becomes ever clearer as scientific knowledge about this complex link continues to evolve.
We’re now on WhatsApp. Click to join.
Like this post?
Register at One World News to never miss out on videos, celeb interviews, and best reads.